Skin Infection
Doctor Instruction:
You are the on-call surgical senior hour officer covering Vascular Surgery and Plastic Surgery. Your next patient is called Lui, who is a 56-year-old man coming in with left leg pain. Please take a history and perform an appropriate examination.
Patient History:
Lui, a 56-year-old male, retired.
Since last week, you have been getting worsening lower left leg pain around the on-going ulcer located at the front of your left lower leg. This ulcer has been there for many years, and the area around it is getting redder and warmer to touch. The skin feels really tense and thickened and looks swollen compared to the other leg.
You are unsure if you have a fever as you don’t own a thermometer at home, but you sometimes shiver with occasional night sweats.
Your appetite has reduced. You do not feel well. You feel tired.
No fluid-filled blisters. No bleeding or discharge. No recent trauma or injury. No insect bites. No recent surgeries or immobility. No nausea or vomiting. No itchiness. The joints are normal. No abnormal sensation. No weakness.
Ideas, Concerns, Expectations:
You have no idea what this might be, but you heard from your friend that this might be something called “?DVT”, which your friend had following a hip replacement in the hospital. You are concerned about this, so you would like to find out what is happening!
Past Medical History:
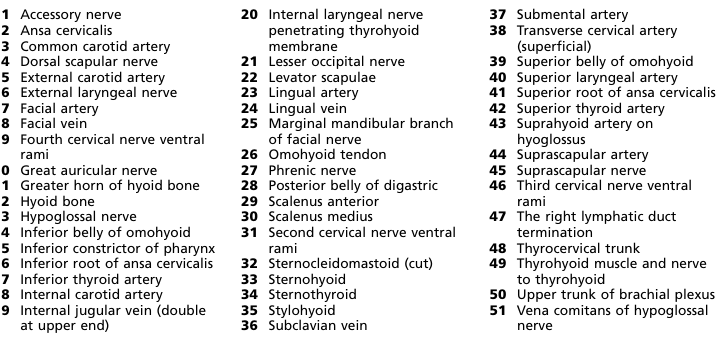
Diabetes, obesity, venous insufficiency, venous ulcer left lower leg, IBD
Drug History:
Metformin, atorvastatin, azathioprine NKDA
Family History:
Diabetes, HTN
Social History:
Drink 2-4 cans of beer a night.
No recreational drug use.
Non-smoker.
Live alone in a Bungalow – you will often have district nurses around for wound care of your ulcer for the past few years.
Retired.
Examination Findings:
Venous ulcer at anterior left lower leg with surrounding warm and tender erythematous skin. Poorly demarcated redness. No skin crepitus. No blisters or vesicles. Varicose veins can be seen in both lower legs.
No necrotic / gangrenous tissues. No pitting oedema. No toe-web abnormalities. – e.g. fissures, scaling, maceration. No injury/trauma site. Neurovascular intact. CRT < 2seconds.
Differentials:
Cellulitis
Erysipelas
Rule out DVT
Rule out pyoderma granulosum/ necrotising fasciitis
Superficial thrombophlebitis
Varicose eczema
Investigations:
Cellulitis can be diagnosed clinically.
Consider wound, skin swab/blood culture/aspiration/biopsy if appropriate.
Consider referral to be seen at the hospital and for bloods if the patient is systemically unwell: FBC, CRP, U&E, LFT, Bone Profile, culture and perform sepsis 6
Consider assessing diabetic control: BM, serum glucose, hba1c
Consider XR, USS, or MRI for assessing the spread of infection, e.g. bone, gas in subcutaneous tissue, abscesses, or involving foreign bodies…etc., at the hospital.
Management:
Conservative:
Rest, elevation of affected limb and analgesia, e.g. paracetamol/ NSAID / opioid.
Hydration
VTE prophylaxis/assessment
Clean affected site: irrigation, debride devitalised tissues if appropriate.
Emollient to moisturise skin
Imaging/drawing to assess the progression of spread/resolution with follow-up.
Assess tetanus risk and status if punctured wound or laceration
Safety netting if non-improving or worsening symptoms/ signs 48 hours after the course of antibiotic
Medical:
Consider hospital admission for severe cellulitis, immunocompromise, significant comorbidity, social issues, systematic illness, non-responsive to oral treatment, further deterioration, necrotising fasciitis, and orbital cellulitis.
Consider referral to dermatology, surgery, or other specialists if appropriate for urgent review or advice.
Flucloxacillin (Oral/IV), alternative: erythromycin, clarithromycin, clindamycin, doxycycline, co-amoxiclav.
If MRSA is suspected, consider adding one of vancomycin, teicoplanin or linezolid to standard treatment.
Long-course antibiotics for patients with lymphoedema until signs of acute inflammation have resolved – may take 1-2 months.
Course otherwise is generally for seven days and can be extended to 10-14 days to ensure complete resolution.
Surgical:
If presenting crepitus/ necrotic appearing skin, this requires urgent surgical intervention to exclude necrotising fasciitis. Crepitus also requires urgent debridement of tissue. If symptoms or signs of osteomyelitis, or septic arthritis, this requires urgent orthopaedic input.
Prevention:
Good diabetic control
Good wound/ulcer management: regular use of absorbent but non-adhesive dressing, aspirate / deroof blisters using aseptic technique as per local protocol
Weight control
Treatment of athlete’s foot if present
For chronic limb swelling: elevation, calf muscle exercises, compression stockings (only when acute cellulitis has resolved)
Appropriate footwear, treat neuropathy in diabetes and avoid injury to the skin.
Consider antibiotic prophylactics for recurrent cellulitis under specialist guidance, e.g. phenoxymethylpenicillin 250mg BD/ erythromycin 250mg BD.
Viva Questions:
Explain the pathophysiology of cellulitis.
Cellulitis is caused by bacteria entering the skin through cuts, bites, or breaks. These bacteria trigger an immune response, causing inflammation, redness, swelling, and pain. Immune cells gather to fight the infection, leading to widened blood vessels and fluid leakage into the tissue (edema). This process can damage the surrounding tissue. If the infection spreads through lymphatic vessels, red streaks may appear, and nearby lymph nodes can become swollen.
What are the risk factors of cellulitis?
Skin breaks (cuts, bites).
Weakened immune system.
Impaired circulation.
Lymphatic issues.
Chronic skin conditions.
Obesity.
Prior cellulitis.
IV drug use.
Age-related factors.
Unhygienic conditions.
Trauma.
What are the common pathogens associated with cellulitis?
Staphylococcus aureus (including MRSA).
Streptococcus pyogenes.
Other Streptococci.
Other Staphylococci.
Haemophilus influenzae (less common).
Gram-negative bacteria (in specific cases)
What is the Eron Classification for assessing the severity of cellulitis?
ree
What are the complications of cellulitis?
Abscess formation.
Bacteremia (bacteria in bloodstream).
Lymphangitis (infection spreads via lymphatics).
Lymphadenitis (swollen lymph nodes).
Necrotizing fasciitis (rare, severe tissue infection).
Sepsis (systemic infection).
Chronic cellulitis recurrence.
Functional impairment and scarring.